What is a WBA?
WBA is a form of authentic assessment that tests performance in the real environment that doctors face in their everyday clinical practice. WBA should enable international medical graduates to demonstrate their progress in integrating clinical knowledge and skill as a basis for effective clinical judgments and decisions. It should also track their development towards becoming an independent, self-monitoring clinical practitioner in the Australian setting, which includes effective communication, respect for patients, working productively within a team of healthcare professionals, and applying risk-management skills.
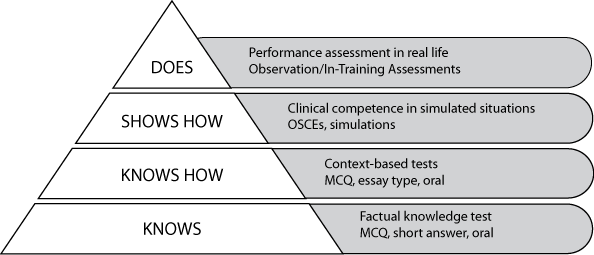
How this form of assessment relates to other forms of assessment is clarified by reference to Miller’s Pyramid. In 1990 Miller used a pyramid to provide a framework for clinical assessment which is shown at Figure 1. Relative to the levels of assessment in Miller’s Pyramid, written examinations assess candidates at the ‘knows’ and ‘knows how’ levels, and clinical assessments assess at the ‘shows how’ and ‘does’ levels. WBA is an assessment at the ‘does’ level, as its focus is on performance in the workplace setting.
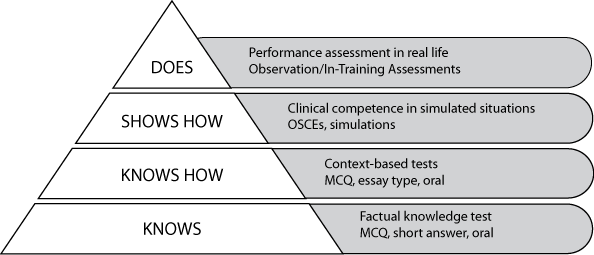
The AMC CAT MCQ examination is at the ‘knows how’ level of the pyramid which tests clinical decision-making skills and the ability to apply knowledge to clinical problems.
The clinical examination is in an Objective Structured Clinical Examination (OSCE) format. It is at the ‘shows how’ level, as it assesses candidates’ ability to perform in simulated situations.
WBA measures what a doctor does in practice.2,3 WBA contributes important information about overall suitability for independent practice in Australia.